Description
Humeral Stem
Positioned approximately 12mm below the resected humeral neck osteotomy to ensure that the humeral socket is surrounded by proximal bone support for strength, stability and fixation.
- Anatomical-shaped proximal body
- Cylindrical-shaped distal segment with cement flutes
- Cemented application only
- Primary stem: 6 x 101mm, 7 x 105mm, 8 x 109mm, 10mm x 116mm, and 12mm x 124 mm
- Revision sizes: 6mm, 8mm, 10mm, and 12mm in one length of 175mm

Humeral Socket
Stabilizes the superior and medial pulling forces of the deltoid muscle to restore joint mobility and minimize the risk of bone erosion caused by impingement of the humeral socket against the inferior aspect of the glenoid.
- Morse taper fixation to the humeral stem
- Shell sizes: neutral, +4mm offset, and +8mm offset
- 18 different sizing configurations
- Insert sizes: 32mm, 36mm, and 40mm in both standard and semi
- Titanium alloy constrained option

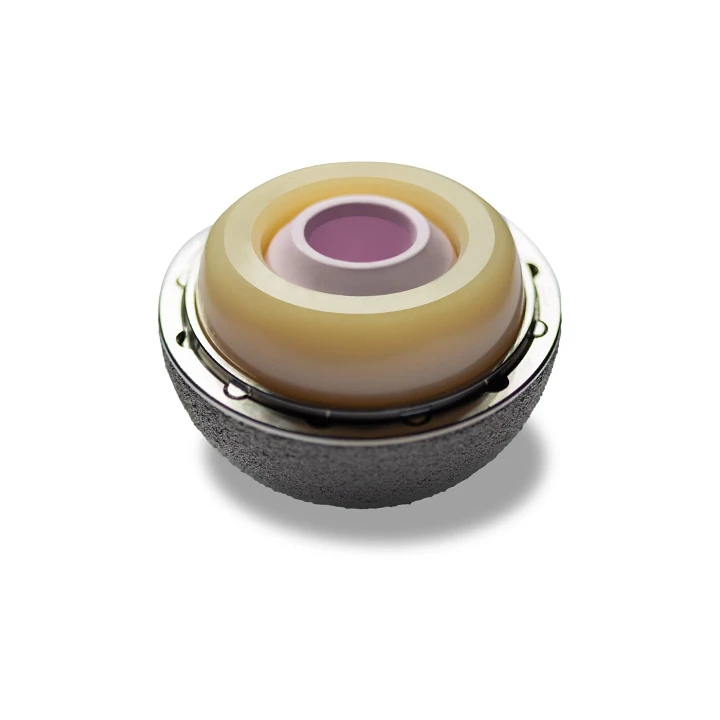
Glenoid Head
Delivers a force of resistance against humeral socket/glenoid head combination to prevent superior escape of the humerus for long-term stability and wear characteristics.
- Reverse Morse taper fixation to the glenoid baseplate
- Sizes: 32mm, 36mm, and 40mm available in neutral or -4mm offset
- 3.5mm titanium alloy retaining screw mates into glenoid head for additional security

Glenoid Baseplate
Centralized 6.5mm cancellous bone screw with four peripheral 5.0mm locking or 3.5mm non-locking cortical bone screws deliver outstanding fixation and long-term stability.
- Hydroxyapatite coating plasma sprayed over 3DMatrix® porous coating
- 5.0mm locking cortical bone screws for perpendicular placement
- 3.5mm non-locking cortical bone screws for angled placement in any direction up to 12 degrees
- 26mm diameter baseplate in one length of 30mm
Clinical Challenge
Patients presenting with an irreparable, rotator cuff deficient shoulder joint with severe arthropathy typically show evidence of an upward displacement of the humeral head with respect to the glenoid and a loss of glenohumeral joint space. Unfortunately, the functional outcomes using conventional surgical methods are severely limited and typically fail.
Clinical Solution
The Reverse® Shoulder Prosthesis is a semiconstrained design concept that reverses the shoulder anatomy by lateralizing the shoulder joint to effectively resist the superior pull of the deltoid muscle and optimize soft tissue balancing.
Indications
- Grossly rotator cuff deficient shoulder joint with severe arthopathy;
- A previously failed joint replacement with a grossly rotator cuff deficient shoulder joint;
- Evidence of upward displacement of the humeral head with respect to the glenoid;
- Loss of glenohumeral joint space
Biomechanical Evaluation of the Reverse Shoulder
Background
- In patients with rotator cuff arthropathy, a “reverse” shoulder prosthesis resists glenohumeral subluxation and offers the potential for improved function.
- Premature mechanical failure due to loosening of the glenoid component is a concern with these devices, especially when used in revision shoulder arthroplasty and in patients with less-than-optimal bone stock, as some reverse shoulder prosthesis have increased lateral offset at the glenohumeral articulation with potentially greater loads transferred to the bone-prosthesis interface.
- The potential clinical advantages for using an increased offset reverse shoulder prosthesis, such as enhanced stability and function, can only be realized if satisfactory glenoid component fixation is achieved.
In-Vitro Study
- In-vitro study evaluated initial glenoid component fixation of 2 uncemented “reverse” prostheses during physiologic loading to determine the relationship among lateral offset of the glenosphere, fixation method, and motion.
Results
- Both lateral offset and peripheral screw type affected the magnitude of baseplate motion.
- Baseplate motion for Delta III components and Reverse® Shoulder Prosthesis components fixed with 5.0mm captured screws were below the 150 μm of motion generally accepted as the threshold for bone ingrowth.
- Stable fixation was achieved for the Reverse Shoulder Shoulder Prosthesis neutral components despite a substantially (69%) greater moment at the baseplate-foam interface compared with the Delta III.
Herman M, Frankle M, Vasey M, Banks S. Intial Glenoid Component Fixation in “Reverse” Total Shoudler Arthroplasty: A Biomechanical Evalutation. Journal Shoulder Elbow Surgery. 2005 Jan/Feb; 14(15): 1625-1675
Consulting Shoulder Design Surgeon – Mark Frankle, M.D.
One of DJO Surgical’s leading and most influential key design surgeons is Mark A. Frankle, M.D. as he developed the Reverse® Shoulder Prosthesis and is instrumental in the continued development of the system.
Dr. Mark A. Frankle has been with Florida Orthopaedic Institute, Tampa, Florida, since 1991. He attended Rush University College of Medicine after completing three years of undergraduate studies at Grinnell College in Iowa. Dr. Frankle completed his residency training at the University of South Florida. After residency, he completed an orthopedic pathology and orthopedic implants fellowship at Rush-Presbyterian St. Lukes Hospital. He then completed a reconstructive technique research fellowship program at the prestigious AO/ASIF Prosthetic/Implant Research and Development Complex in Davos, Switzerland. Dr. Frankle then completed an adult reconstructive surgical fellowship at the Mayo Clinic in Rochester, Minnesota.
Dr. Frankle serves as the Director of the Biomechanical Shoulder and Elbow Research Lab at the University of South Florida College of Engineering and is the Director of the annual course, “Current Concepts in Shoulder and Elbow Surgery.” He has published numerous articles in professional journals and maintains ongoing research projects, presenting his work annually at various professional conferences. Dr. Frankle has designed implants and instrumentation used in shoulder replacement for several different orthopedic companies. Dr. Frankle received the prestigious Charles S. Neer Award for Basic Science from the American Academy of Orthopaedic Surgeons. Dr. Frankle is board-certified by the American Board of Orthopaedic Surgery and a member of the American Shoulder and Elbow Society.





Reviews
There are no reviews yet.